Post Graduate Diploma in Public Mental Health
Mental illnesses are rising and have a widespread impact on functioning across one’s lifespan. These illnesses affect not only individuals but families and societies. Recent rapid societal transitions can cause an excessive burden on individuals, stigma, and a lack of help. Low and middle-income countries are facing new challenges in dealing with the increased prevalence of anxiety and
depression in younger age groups in the recent COVID-19 pandemic. Mental health is a public health issue concerning national and international development and security. In low- and middle-income countries LMICs),
most persons with mental and substance use disorders lack access to decent services and effective interventions; the so-called "treatment gap" is estimated to be more than 75-86% in LMICs. The main reasons for this glaring treatment gap are stigma and discrimination associated with MNS disorders, institutional models of cases prevalent in most LMICs, and irrational use of scarce human and financial resources. In order to bridge this treatment gap, the Mental Health Gap Action Program, or mhGAP, was launched by WHO in 2008. It aims to scale care for priority mental, neurological, and substance use conditions, particularly in poorly resourced settings. It delivers integrated packages of evidence-based interventions through primary health care services. Critical strategies for delivering mental health interventions identified include stepped care, task sharing with appropriately trained and supervised non-specialist workers and collaborative care. The 66th World Health Assembly adopted the comprehensive Mental Health Action Plan 2013– 2020 to set a vision and roadmap for mental health for countries worldwide to achieve by 2020. It identifies specific actions for Member States and international and national partners with agreed targets and indicators. In order to initiate the vision and roadmap set out in the plan, member states of the Eastern Mediterranean region implemented a regional framework for scaling up action on mental health in the 62nd meeting of the Regional Committee in 2015. The regional framework identifies critical strategic interventions across governance, health services, promotion and prevention, surveillance, monitoring, and research. It also provides a set of indicators to monitor progress in implementing these interventions. One of the critical interventions identified in the regional framework is to enhance the capacities of family physicians and general practitioners to recognize and manage priority MNS disorders identified in mhGAP to scale up mental health care in countries of the region. Several challenges in light of the experience of implementing this strategic intervention, including the need for regular supportive supervision and referral support. This particular challenge is not only due to a shortage of specialist workforce, paucity of financial resources, logistics, and administrative difficulties but also to security concerns in several regional countries. In order to address these challenges, we are proposing to develop a cadre of family physicians and mental health professionals who can provide not only mental health care within PHC settings but also provide supervisory and referral support to their peers and act as a middle layer of between specialists and health care workers to bridge the gap, and provide quality mental health care to the people. The main aims of the training modules of this diploma are detailed assessments of common mental disorders and ethical practice of evidence-based clinical psychiatry. This diploma course's further objectives are to prevent mental illnesses and promote mental well-being.
Project Length
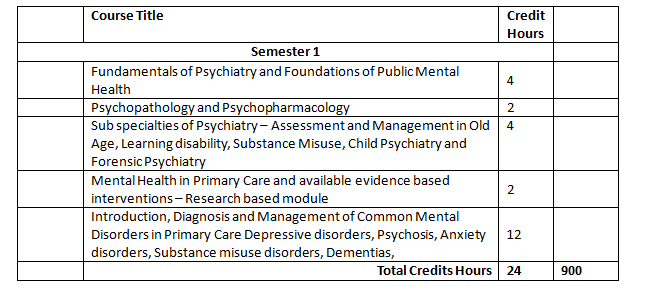
It is a One-Year program comprising of 2 semesters and each semesters’ duration is 16 weeks.
Methods of Assessment/Examination, Procedures and Rules:
Students will be evaluated during each course on the basis of
1. Formative assessment: which is a mix of the tests, end of course examination, class and home assignments, class participation, interactive discussions, practical exercises, field works and/or group works, end of course examination, depending on the course outline (ongoing assessment);
2. Summative assessment: based on the end of semester examination papers. Summative assessments are held at the end of semesters and comprises of semester examinations paper each.
1. Formative assessment: which is a mix of the tests, end of course examination, class and home assignments, class participation, interactive discussions, practical exercises, field works and/or group works, end of course examination, depending on the course outline (ongoing assessment);
2. Summative assessment: based on the end of semester examination papers. Summative assessments are held at the end of semesters and comprises of semester examinations paper each.
Anyone who has completed a bachelor’s Degree in medicine, psychology, nursing, and public health will be entitled to admission. This diploma will be available nationally and can be attended remotely. 2-4 weeks’ attachments will be carried out in the tertiary hospitals. Non-medical graduates may opt to study for six months to achieve Post Graduate Certificate in Public Mental Health, in this certificate 60 hours classroom teaching and three months clinical placement at collaborating institutes of Mental Health of Health Services Academy which are across the country
Age Limit
There is no Age-limit restrictions for admission in this Program.
Course Fee is Rs. 60,000 per semester.
Total fee for One Year Diploma is Rs.120,000 which is payable in two instalments.
International Students: USD 1000
Total fee for One Year Diploma is Rs.120,000 which is payable in two instalments.
International Students: USD 1000